Only 13% of people report having good mental health, according to a 2017 survey by the Mental Health Foundation.
Mental health isn’t all or nothing, it exists on a continuum that changes over time.
We all have mental health, and like physical health, it needs time, care and attention.
When it comes to what we eat, we need to shift the conversation towards how we feel as a sign of health (rather than just shape or size).
So, can what you eat make a difference to your mood?
What we’ll cover today:
How what we eat can shape our mood
The effects of fibre, lifestyle and probiotics on mental health
10 small, practical steps to thrive each day
New research insights: Could these foods boost mood? (and 4 ways to eat more of them) (paid subscribers)
Can what you eat boost your mood?
There is growing good-quality evidence that improving your diet can help improve your mood.
I’m going to highlight two meta-analyses (1, 2), that found that when people with depression followed healthier eating patterns (especially those similar to a Mediterranean-style diet) they experienced a noticeable lift in their symptoms.
These studies looked at randomised controlled trials (the gold standard of study design), where people were randomly assigned to change their diet, often with the help of a dietitian.
On average, those in the diet change groups reported significantly fewer depressive symptoms than those who didn’t change their eating habits.
How to support your own mental well-being?
Think about what you can add in - like a handful of fresh berries with breakfast, a chickpea and tomato salad for lunch, or grilled fish with herby whole grains for dinner.
It’s not about perfection, it’s about small shifts towards colourful, fibre-packed foods that your brain (and gut) will thank you for.
How what you eat affects how you feel
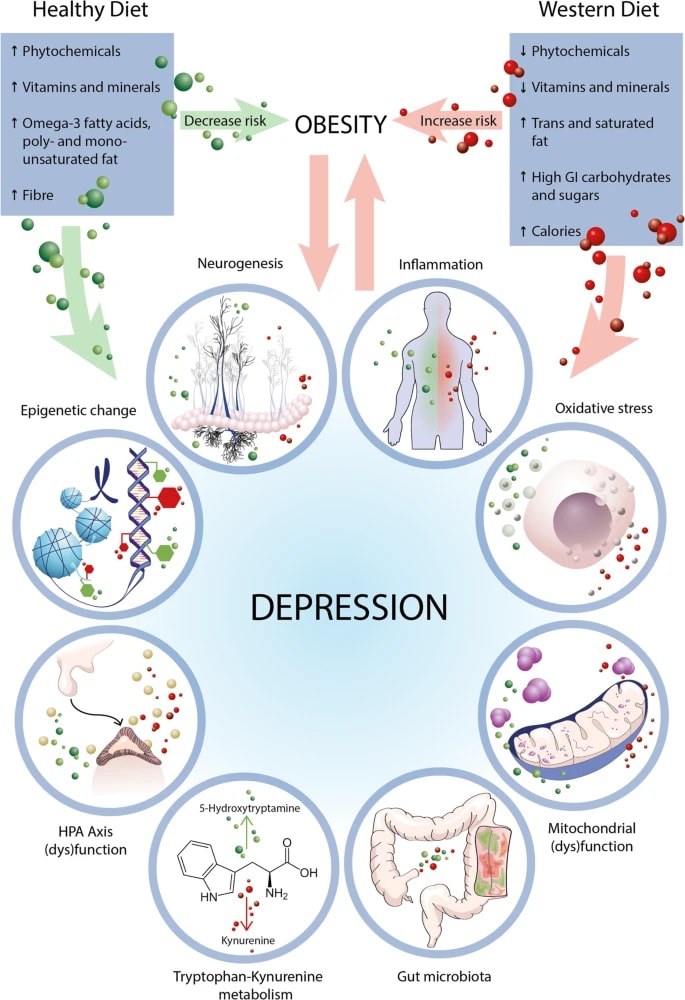
Scientists are uncovering several potential biological pathways that may help explain the link between diet and mood.
Most of this research is still early-stage or based on animal studies, but it gives a first peak into some of the ways what we eat influences how we feel:
Inflammation and oxidative stress: Eating a poor diet might trigger low-grade inflammation and oxidative stress (that may lead to cell damage over time), which have been linked to low mood.
Gut health: The food we eat shapes our gut microbes - and they talk to the brain. These microbes might affect our mood by influencing things like our immune system, hormones and nerves.
Stress system (HPA axis): What you eat may help calm the body’s stress response. This system is often overactive in people with depression.
Brain plasticity (BDNF and neurogenesis): In animal studies nutrients like omega-3s and polyphenols may support brain cell growth and connections, which is often lower in depression.
Tryptophan pathway: This amino acid helps make serotonin, one of our “feel-good” brain chemicals. But if there’s too much inflammation, it can get rerouted into making other compounds that aren’t so helpful for mood, like quinolinic acid.
Energy production (mitochondria): Our brain cells rely on tiny energy factories called mitochondria to work properly. Poor diet may disrupt how they produce energy, and this has been linked to symptoms like fatigue and brain fog, especially in depression.
Early life and gene expression: What we eat early in life (or even what our parents ate) can shape how our brain develops. This may be due to epigenetic changes, which influence how genes are turned on or off.
What we eat doesn’t just keep us going - it also may shape how we feel, think and cope.
Can fibre lift your mood?
A 2024 meta-analysis pulled together findings from 23 studies that looked at the link between how much fibre people eat and their mental health, in the real world.
The researchers also looked at 10 clinical trials where people were given fibre supplements to see if they made a difference to their mood.
In the observational studies, people who ate more fibre generally reported fewer symptoms of depression and anxiety. The effect was small, but it was there.
But when it came to the clinical trials (where people took fibre supplements) the results weren’t as convincing. Overall, taking fibre supplements didn’t make a noticeable difference to mood or anxiety compared to a placebo.
It’s worth noting that all of the clinical trials used isolated fibre supplements, not fibre from whole foods, which come bundled with other nutrients, polyphenols and other plant compounds that may work together to support mental health.
So while fibre supplements alone might not lift your mood, a diverse, whole food fibre-rich diet still might.
Feeling better through food and movement
The CALM trial looked at whether a lifestyle-based approach (focusing on improving diet and increasing movement) could work nearly as well as traditional talk therapy (CBT) for people with depression.
Both treatments were delivered online in small groups over eight weeks. The lifestyle sessions were led by dietitians and exercise specialists, supporting people to make small, realistic changes to their eating and physical activity.
This was what’s called a non-inferiority trial, meaning the goal wasn’t to prove lifestyle therapy was better, just that it wasn’t meaningfully worse than CBT.
And people in both groups saw similar improvements in their depression symptoms.
That’s important because it means lifestyle changes can play an active part in our mental well-being, that can complement talking therapy.
Can probiotics beat the blues?
A 2024 network meta-analysis looked at how probiotics stack up against antidepressants for treating depression, with encouraging findings.
This type of analysis lets researchers compare lots of treatments, even if they haven’t all been tested against each other in the same trial.
Probiotics were found to significantly lower depressive symptoms compared to a placebo. They ranked just behind escitalopram (a common antidepressant) and even came out ahead of several others - but the level of certainty was either low or very low, so we do need to be cautious.
Most of the studies tested probiotics taken alongside antidepressants rather than on their own. So while they might still help solo, the evidence mainly supports using them as an add-on, not a replacement.
Which probiotic type is best? Comparing probiotics across studies is tricky. Each one used different strains, doses, and combinations. So based on this study, we don’t know which type is necessarily ‘better’.
Certain probiotics may help by influencing neurotransmitters like serotonin and GABA, calming low-grade inflammation, and supporting the gut barrier - all key parts of the gut-brain connection.
10 steps to thrive
Talk about your feelings: Opening up isn’t a sign of weakness. Sharing how you feel helps you manage tough times and stay mentally healthy.
Keep active. Exercise helps your brain and mood. It doesn’t have to be intense - walking, gardening, or housework all count.
Eat well: Your brain needs good nutrition, and hydration. Try for a varied diet with plenty of fruits, vegetables, whole grains, nuts, seeds, oily fish, and water.
Drink sensibly: Even drinking occasionally isn’t ideal for your mental well-being, though we have to recognise that being social is - and alcohol often comes as a part of that. Stick to low alcohol or no-alcohol options to protect your mood and health.
Keep in touch: Strong relationships support your mental health. Stay connected with friends and family, even if it’s just a call or message.
Ask for help: If you’re struggling, don’t hesitate to reach out, whether to your GP, a specialist, or in an emergency, seek support.
Take a break: Pause when you need to. A short rest, a change of scene, or some quiet time can recharge your mind and body.
Do something you’re good at: Hobbies and activities you enjoy boost your mood and confidence. Take time for yourself outside your roles and responsibilities.
Accept who you are: Focus on your strengths and accept your uniqueness. Realistic goals and self-acceptance help build resilience.
Care for others: Helping others can improve your own wellbeing. Volunteering or supporting those close to you can boost your confidence and sense of purpose.
This advice is adapted from the Mental Health Foundation’s “10 Ways to Look After Your Mental Health” guide.
Keep reading with a 7-day free trial
Subscribe to Second Brain to keep reading this post and get 7 days of free access to the full post archives.